ESC Congress 2019
Several researchers presented their latest studies at the annual Congress of European Society for Cardiology, the largest get-together of its kind. Elevating the Congress further this year was its conjunction with the World Congress of Cardiology, putting the spotlight on global cardiovascular health, highlighting differences in prevalence, clinical manifestations, prevention strategies, diagnostic modalities and management of cardiovascular diseases around the world, as stated on the ESC webpage.
Our research collaborator in Japan, assistant professor Katsuji Inoue, MD, PhD, presented two very interesting studies, the first suggesting that left atrial reservoir strain can be used to predict elevated pulmonary capillary wedge pressure, thus allowing discrimination between pre- and post-capillary pulmonary hypertension. The second study “Estimation of pulmonary artery pressure from right atrial strain and tricuspid regurgitation velocity” concluded that right atrial strain provides a semiquantitative measure of right atrial pressure, which can be used in combination with peak tricuspid regurgitation velocity to estimate systolic pulmonary artery pressure. This approach can be used as an alternative when the IVC method (estimation of right atrial pressure by echocardiographic evaluation of inferior vena cava diameter and collapsibility) is not available in cases with poor subcostal window.
Dr. Inoue also co-authored the study «Restricted left atrial motion as a result of atrial stiffening in patients with cardiac amyloidosis” that sought to determine whether left atrial (LA) reservoir strain with speckle tracking echocardiography could be used as a marker of LA stiffness in a derivation cohort. Furthermore, the hypothesis that LA reservoir strain could differentiate cardiac amyloidosis (CA) patients from hypertrophic cardiomyopathy (HCM) in an independent validation cohort was tested. The study concluded that LA reservoir function was fairly limited in patients with CA compared with HCM. Restricted LA motion might be related to atrial amyloid deposits or fibrosis, which potentially provokes atrial chamber stiffening.
State of the Art in diastolic function assessment
Speaker: Otto A. Smiseth, ESC Congress 2019, Paris, France
The importance of diastolic function has become evident as heart failure has become epidemical across the globe; 1 million patients are hospitalized annually in the USA alone. Approximately half of them have an ejection fraction above 50%, which has led to the need of easily available measures for LV filling pressure.
Demonstration of elevated left ventricular filling pressure at rest or exercise is conclusive evidence of heart failure with preserved ejection fraction (HFpEF). Left ventricular filling pressure at rest can be estimated with high feasibility and good accuracy by echocardiography. Left atrial reservoir strain appears useful when the study is nonconclusive with conventional echo indices.
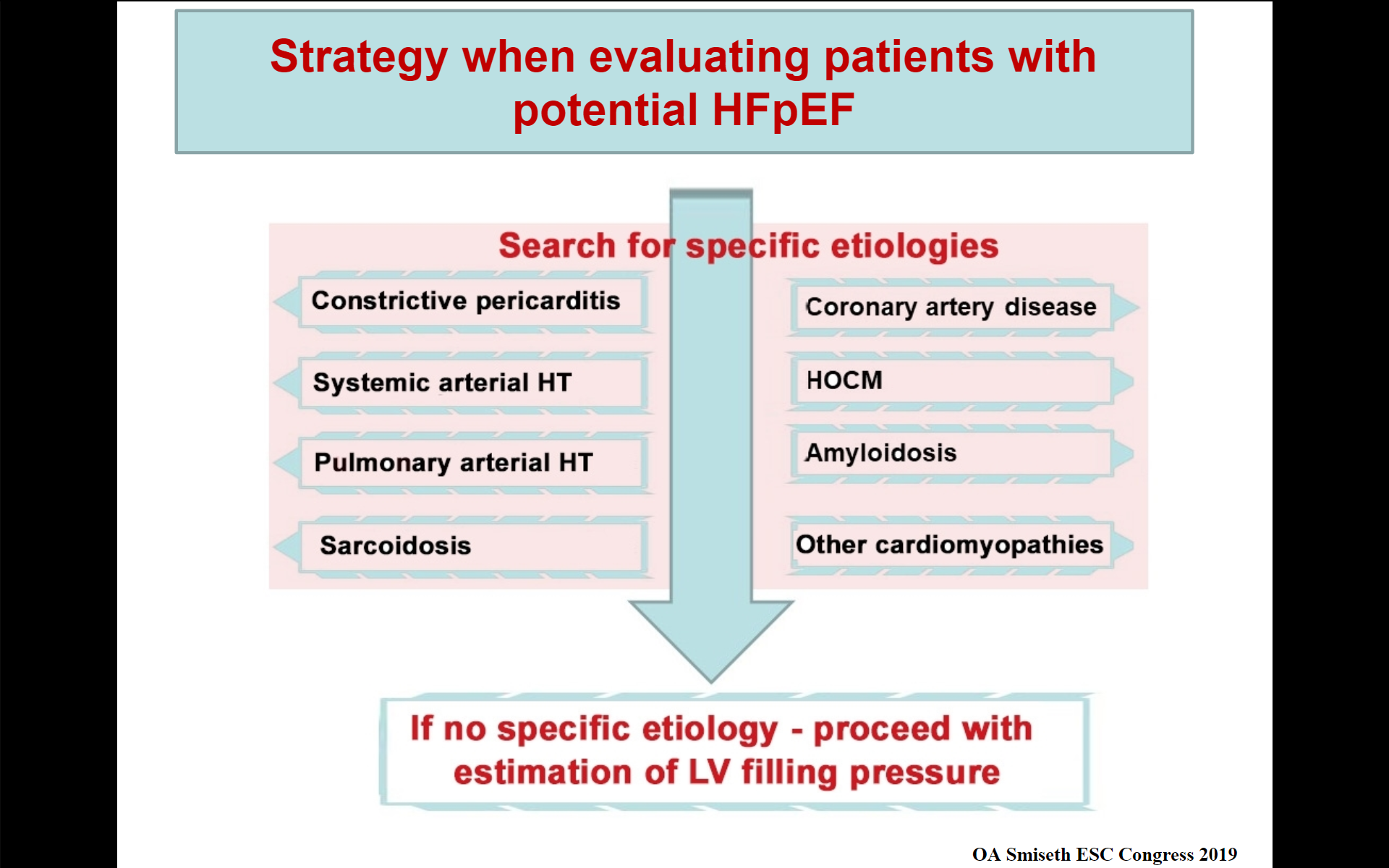
When evaluating patients for potential HFpEF it is important to search for specific etiology. Always measure left ventricular global longitudinal strain, since its reduction confirms LV dysfunction.
The study by PhD fellow Faraz Khan, MD & co concluded that left atrial strain may have a role in non-invasive estimation of left ventricular filling pressure, particularly in patients who remain unclassified when using the conventional echocardiographic indices.
PhD fellow John Aalen, MD, & co looked into cardiac resynchronization therapy (CRT) in their study “Septal function and viability determine response to cardiac resynchronization therapy“. CRT has evolved as an important treatment in patients with symptomatic heart failure, reduced left ventricular (LV) ejection fraction and wide QRS. However, as one third of patients do not benefit from the therapy, there is need for better selection criteria. Previous studies have shown an association between recovery of septal function and response to CRT. A multimodality approach with strain echocardiography and LGE-CMR was able to detect CRT responders with high accuracy, also in the subset of patients with intermediate QRS duration. A dysfunctional but viable septum appears to be an ideal target for CRT.
PhD fellow Camilla Larsen, MD & co investigated the ability of advanced echocardiographic and nuclear imaging techniques to detect septal and left ventricular (LV) lateral wall scar in patients referred for CRT, compared to late gadolinium enhancement (LGE) cardiac magnetic resonance. The study concluded that septal negative work correlates inversely with septal scar in patients referred for CRT. This finding is probably linked to LBBB, and may be explained by increased stiffness of scar tissue. Myocardial work, but not peak strain, reflects scar in the LV lateral wall. Future studies should explore the assessment of scar in the complete LV and how this relates to CRT response.
Abstracts presented at ESC Congress 2019:
Authors: K Inoue, EW Remme, FH Khan, OS Andersen, E Gude, H Skulstad, OA Smiseth
Institute for Surgical Research, Oslo University Hospital, Rikshospitalet, Oslo, Norway
Background: Pulmonary hypertension (PH) is classified as pre- or post-capillary PH, and pulmonary capillary wedge pressure (PCWP) > 15 mmHg is used as criterion for post-capillary PH. Elevated left atrial (LA) pressure is associated with reduced LA reservoir strain. Thus, LA strain may potentially serve to differentiate between these diagnoses.
Objectives: This study tested the hypothesis that LA strain can be used as a noninvasive parameter to differentiate between pre- and post-capillary PH.
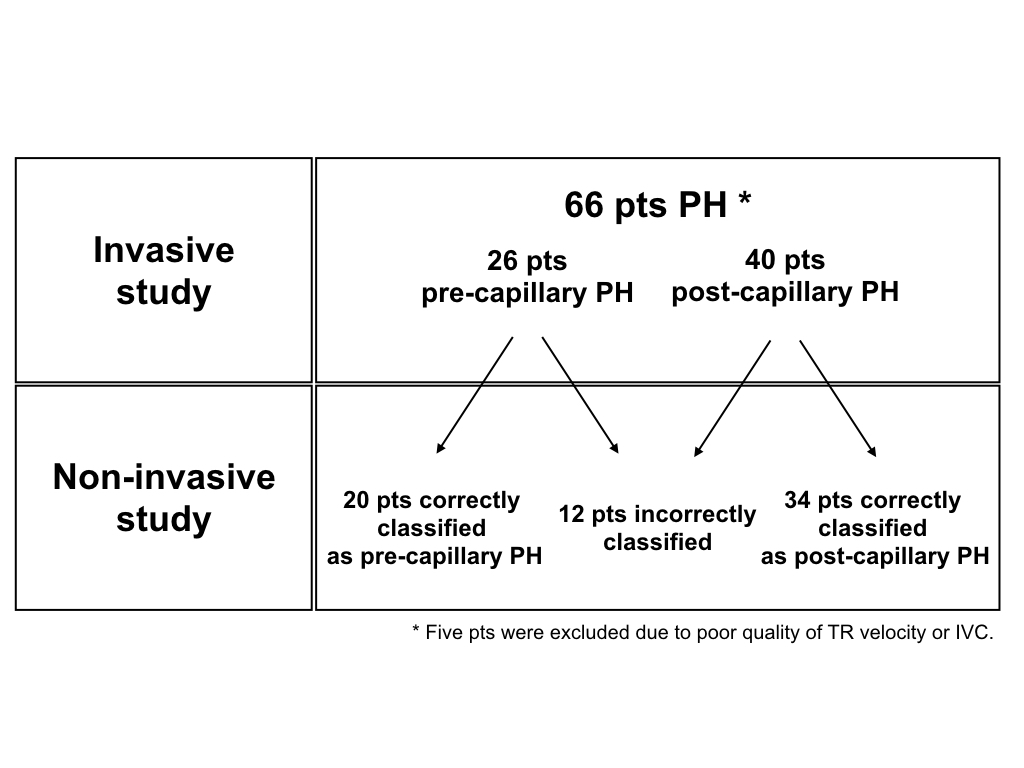
Methods: We analyzed 103 patients (mean age: 58 years, 51 female) referred to right heart catheterization due to unexplained dyspnea or suspected heart failure. Echocardiography was performed within 24 hours of the invasive procedure. Mean pulmonary artery pressure (PAP) was noninvasively estimated from tricuspid regurgitation (TR) velocity and inferior vena cava (IVC) diameter and collapsibility. LA reservoir strain was calculated from apical four-chamber view by speckle tracking echocardiography, and was feasible in 101 patients.
Results: Twenty-eight patients were invasively confirmed with pre-capillary PH and 43 patients with post-capillary PH. The remaining 32 patients had no PH. LA reservoir strain was significantly lower in patients with post-capillary PH than patients with pre-capillary PH (9.9 ± 5.5% vs. 24.6 ± 8.2%, p< 0.01). At a cut-off value of 15.4%, LA reservoir strain could predict elevated PCWP > 15 mmHg with AUC=0.88, sensitivity=84.8% and specificity=81.8%. As shown in the figure, echocardiography with LA reservoir strain correctly differentiated 82% of patients into pre- and post-capillary PH.
Conclusions: These results suggest that LA reservoir strain can be used to predict elevated PCWP, thus allowing discrimination between pre- and post-capillary PH.
Inoue K, Remme EW, Khan F, Andersen OS, Gude E, Skulstad H, Smiseth OA
Institute for Surgical Research, Oslo University Hospital, Rikshospitalet, Oslo, Norway
Background: Systolic pulmonary artery pressure (SPAP) can be estimated non-invasively as the sum of indices for right atrial (RA) pressure and tricuspid regurgitation (TR) pressure gradient. Although echocardiographic evaluation of inferior vena cava (IVC) diameter and collapsibility is currently being used to estimate RA pressure, RA strain may be an alternative since atrial strain is related to atrial pressure.
Objective: We tested if RA strain by speckle tracking echocardiography can be used as a surrogate of mean RA pressure (RA strain method), and by adding the TR pressure gradient, be used to estimate SPAP.
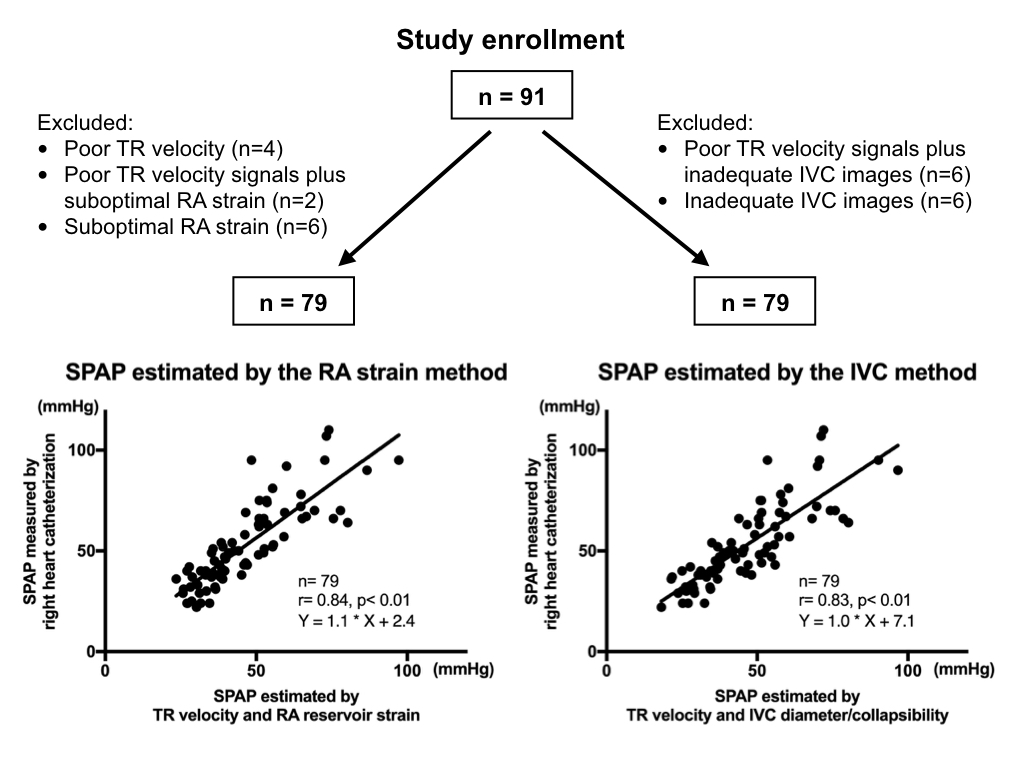
Methods: We retrospectively analyzed 91 patients (mean age, 58 years) referred to right heart catheterization due to unexplained dyspnea or suspected pulmonary hypertension. Echocardiography was performed within 24 hours of the invasive procedure. RA reservoir strain was calculated from apical four-chamber view. SPAP was calculated as the sum of the TR pressure gradient and estimated RA pressure by the IVC or RA strain methods.
Results: Right heart catheterization showed SPAP and mean RA pressures of 51 ± 20 mmHg and 9 ± 6 mmHg, respectively. RA reservoir strain was inversely correlated with mean RA pressure (r= -0.61, p< 0.01). Thus, we set mean RA pressure as 5, 10 and 15 mmHg depending on high (>25%), middle (10-25%) and low (<10%) values of RA reservoir strain. As shown in the figure, both the RA strain and IVC methods when combined with peak TR velocity, provided good estimates of invasively measured SPAP.
Conclusions: RA strain provides a semiquantitative measure of RA pressure, which can be used in combination with peak TR velocity to estimate SPAP. This approach can be used as an alternative when the IVC method is not available in cases with poor subcostal window.
Restricted left atrial motion as a result of atrial stiffening in patients with cardiac amyloidosis
Authors: Haruhiko Higashi,* Katsuji Inoue,* Makoto Saito,† Masaki Kinoshita,* Jun Aono,* Shuntaro Ikeda,* Øyvind S. Andersen,‡ Einar Gude,‡ Helge Skulstad,‡ Espen W. Remme,‡ Otto A. Smiseth,‡ Osamu Yamaguchi*
* Division of Cardiology, Department of Cardiology, Pulmonology, Hypertension and Nephrology, Ehime University Graduate School of Medicine, Ehime, Japan.
† Department of Cardiology, Kitaishikai Hospital, Ozu, Japan
‡ Institute for Surgical Research, Oslo University Hospital, Rikshospitalet, Oslo, Norway
Background: Left atrial (LA) involvement of abnormal amyloid fibrils could induce LA dysfunction and stiffening in patients with cardiac amyloidosis (CA). Thus, the assessments of LA function and stiffness might be a potential approach to diagnose CA phenotype among patients with hypertrophied hearts.
Purpose: We sought to determine if LA reservoir strain with speckle tracking echocardiography could be used as a marker of LA stiffness in a derivation cohort. Furthermore, we tested the hypothesis that LA reservoir strain could differentiate CA patients from hypertrophic cardiomyopathy (HCM) in an independent validation cohort.
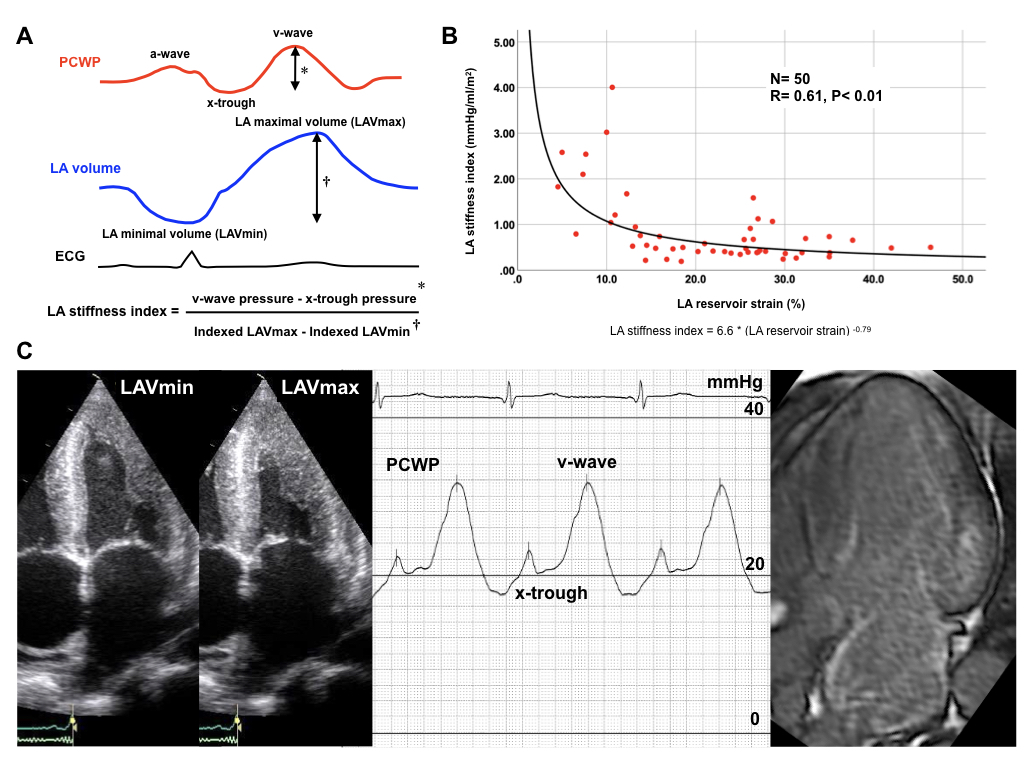
Methods: In the derivation cohort, echocardiography was performed simultaneously with measurements of pulmonary capillary wedge pressure (PCWP) in 50 patients with suspected or established heart failure and relatively preserved left ventricular (LV) ejection fraction (56 ± 10%). LA maximum and minimum volume index, and reservoir strain were measured from apical four-chamber view. LA stiffness index was computed as a pressure rise from x-trough to v-wave divided by an increase from minimum to maximum indexed LA volume (Figure A). In the validation group, we studied a total of 33 biopsy-proved CA patients and 127 HCM patients (LV ejection fraction: 57 ± 11% vs. 66 ± 10%, P<0.01) in sinus rhythm on the date of the echocardiogram. Among them, cardiac magnetic resonance imaging (CMR) could be evaluated in 17 CA patients and 98 HCM patients. Furthermore, right heart catheterization was performed with 12 HCM patients and 12 CA patients in the CMR group.
Results: The derivation cohort study found that there was a significant curvilinear correlation of LA reservoir strain with LA stiffness index (Figure B). In the validation cohort, LA reservoir strain was reduced in patients with CA compared with HCM in all participants (11.6 ± 5.6% vs. 18.5 ± 6.9%, P<0.01), although there was no significant difference of LA maximal volume index between the 2 groups (37 ± 16 ml/m2 vs. 37 ± 12 ml/m2, p=0.89). In the CMR group, late gadolinium enhancement was observed in the LA wall in 16 patients with CA (94.1%) as shown in Figure C. In contrast, the LA enhancement revealed only in 1 patient with HCM (1.0%). Among patients with invasive measures, LA stiffness index [median (interquartile range)] was higher in patients with CA than that in patients with HCM [1.1 (0.4-2.8) vs. 0.2 (0.1-0.6), P=0.01].
Conclusions: LA reservoir function was fairly limited in patients with cardiac amyloidosis compared with hypertrophic cardiomyopathy. Restricted LA motion might be related to atrial amyloid deposits or fibrosis, which potentially provokes atrial chamber stiffening.
Left atrial strain improves estimation of left ventricular filling pressure
Authors: FH Khan1 , OS Andersen1 , E Gude2 , H Skulstad2 , OA Smiseth1 , EW Remme1
1Oslo University Hospital, Institute for Surgical research - Oslo - Norway , 2Oslo University Hospital, Department of cardiology - Oslo - Norway
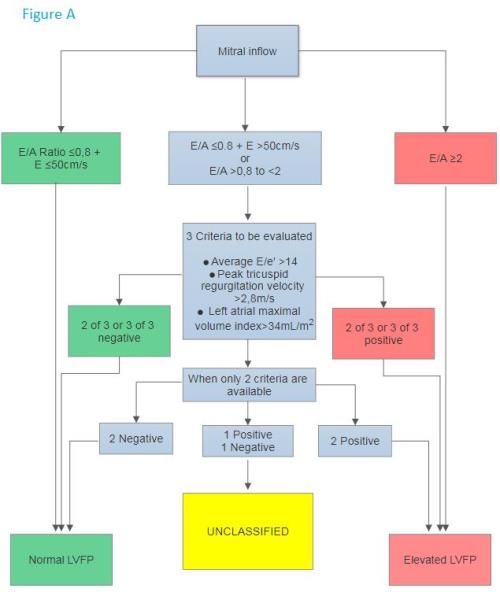
Background: The current algorithm in the 2016 recommendations for echocardiographic estimation of left ventricular filling pressure (LVFP) as normal or elevated, combines traditional indices of mitral inflow velocities, tissue Doppler, left atrial volume and tricuspid regurgitation velocity (Figure A). Some of the patients remain unclassified by this algorithm. Left atrial (LA) strain is a novel index that correlates well with LVFP and may improve estimation of LVFP in these patients.
Purpose: We tested if LA strain can improve estimation of LVFP for the patients that are unclassified by the 2016 algorithm.
Methods: We analyzed data from 100 patients who were referred to right heart catheterization due to unexplained dyspnea or suspected heart failure. Echocardiography was performed simultaneously with or within 24 hours of right heart catheterization. Pulmonary capillary wedge pressure (PCWP) was used as an estimate for LVFP and defined as elevated if above 12 mmHg. Elevated LVFP was first estimated using the 2016 algorithm. In patients who were unclassified by the algorithm due to conflicting indices or unattainable indices, LA strain was subsequently used to detect elevated LVFP using a cut-off found from ROC analysis of the whole cohort.
Results: Six patients were unclassified by the 2016 algorithm. The ROC analysis of all 100 patients showed that at an LA strain cut-off of above or below 16.2%, LVFP was correctly classified as normal or elevated, respectively, with a sensitivity of 83% and specificity of 88%. All 6 unclassified patients by the 2016 algorithm were correctly classified using the LA strain cut-off, effectively increasing the accuracy of the algorithm by 6 percentage points.
Conclusions: LA strain may have a role in non-invasive estimation of LVFP, particularly in patients who remain unclassified when using the conventional echocardiographic indices.
Septal function and viability determine response to cardiac resynchronization therapy
Authors: J Aalen1 , E Donal2 , CK Larsen1 , J Duchenne3 , E Kongsgaard4 , E Hopp4 , M Penicka5 , E Galli2 , JU Voigt3 , OA Smiseth1
1Dep. of Cardiology and Inst. for Surgical Research, Oslo University Hospital - Oslo - Norway , 2University Hospital of Rennes - Rennes - France , 3KU Leuven, Dep. of Cardiovascular Sciences - Leuven - Belgium , 4Oslo University Hospital, Cardiology - Oslo - Norway , 5Olv Hospital Aalst - Aalst - Belgium
Introduction: Cardiac resynchronization therapy (CRT) has evolved as an important treatment in patients with symptomatic heart failure, reduced left ventricular (LV) ejection fraction and wide QRS. However, as one third of patients do not benefit from the therapy, there is need for better selection criteria. Previous studies have shown an association between recovery of septal function and response to CRT.
Purpose: To test the hypothesis that septal dysfunction in the absence of scar predicts response to CRT.
Methods: In 121 patients undergoing CRT implantation according to current European Society of Cardiology guidelines, we performed speckle-tracking echocardiography and estimated LV pressure non-invasively based on a method recently innovated in our lab. Pressure-strain analysis was used to calculate myocardial work. Septal dysfunction with asymmetric LV workload was calculated as the difference between LV lateral wall and septal work. Late gadolinium enhancement cardiac magnetic resonance imaging (LGE-CMR) was performed to assess septal scar. CRT response was defined as =15% reduction of LV end systolic volume by echocardiography at 6 months follow-up.
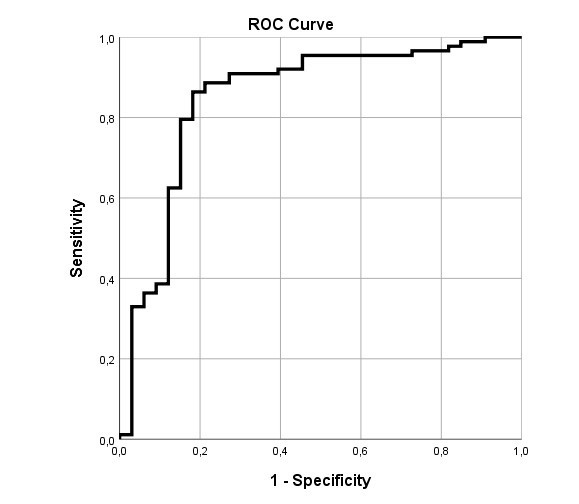
Results: Eighty-eight patients (73%) responded to CRT at 6 months follow-up. Multivariate logistic regression analysis including lateral-to-septal work difference, septal scar, QRS duration and QRS morphology found that only lateral-to-septal work difference and septal scar were significant predictors of CRT response (both p<0.005). Using logistic regression and receiver operating characteristic (ROC) curve analysis, we found that the combined approach of these two parameters identified CRT responders with a sensitivity of 86% and a specificity of 82%. The area under the curve (AUC) for CRT response prediction was 0.85 (95% CI: 0.76-0.94) (Figure). In comparison, the AUC value for QRS duration was 0.63 (95% CI: 0.52-0.75). Furthermore, for the subgroup of patients with QRS duration 120-150 ms (n=27), the AUC value for lateral-to-septal work difference in combination with septal scar was 0.90 (95% CI: 0.78-1.00).
Conclusions: A multimodality approach with strain echocardiography and LGE-CMR was able to detect CRT responders with high accuracy, also in the subset of patients with intermediate QRS duration. A dysfunctional but viable septum appears to be an ideal target for CRT.
Authors: C Kjellstad Larsen1 , E Galli2 , E Hopp3 , J Duchenne4 , JM Aalen1 , G Degtiarova5 , O Gheysens5 , C Stokke3 , JG Fjeld3 , M Penicka6 , J-U Voigt4 , E Donal2 , OA Smiseth1
1Oslo University Hospital, Rikshospitalet, Institute for Surgical Research and Dept. of Cardiology - Oslo - Norway ,2University Hospital of Rennes, Department of Cardiology - Rennes - France , 3Oslo University Hospital, Rikshospitalet, Division of Radiology and Nuclear Medicine - Oslo - Norway , 4University Hospitals (UZ) Leuven, Department of Cardiovascular Diseases - Leuven - Belgium ,5University Hospitals (UZ) Leuven, Department of Nuclear Medicine - Leuven - Belgium , 6Olv Hospital Aalst, Department of Cardiology - Aalst - Belgium
Background: Myocardial scar is frequently present in patients with heart failure and left bundle branch block (LBBB), and associated with reduced response to cardiac resynchronization therapy (CRT). Furthermore, LBBB may be associated with markedly reduced strain, work, metabolism and perfusion in septum, even without septal ischemia. Therefore, it may be challenging to identify scar by functional imaging methods.
Purpose: To investigate the ability of advanced echocardiographic and nuclear imaging techniques to detect septal and left ventricular (LV) lateral wall scar in patients referred for CRT, compared to late gadolinium enhancement (LGE) cardiac magnetic resonance.
Methods: Scar was quantified as percentage LGE in five septal and five LV lateral wall segments of 131 patients (age 66±10, 66% male, QRS-width 164±17ms) referred for CRT, 92% with LBBB. Longitudinal strain was assessed by speckle tracking echocardiography in 130 patients (652 septal and 631 LV lateral wall segments). Myocardial work was calculated by LV pressure-strain analysis. Systolic shortening defined positive work, while systolic lengthening defined negative work. Glucose metabolism was assessed by 18F-fluorodeoxyglucose (FDG) Positron Emission Tomography (PET) in 52 patients (260 septal and 260 LV lateral wall segments). Perfusion was assessed in 46 patients (230 septal and 230 LV lateral wall segments) by either 13N-ammonia PET (n=32) or Single Photon Emission Computed Tomography (SPECT) (n=14). Metabolism and perfusion were reported as percentages of the segment with maximum tracer uptake. We evaluated parameter relationship to scar with Spearman correlation (rs) and regression analysis.
Results: LGE was present in 198 septal (30%) and 136 LV lateral wall (21%) segments. In a multivariate regression model with negative work, metabolism, perfusion and peak strain, only the first three parameters showed a significant association with LGE percent in septum (p<0.001, p=0.022 and p<0.001, respectively), while peak strain did not (p=0.270). Negative work in septum correlated inversely with percentage septal LGE-uptake (rs=-0.33): increasing amount of scar was associated with less negative work (Figure).
In the LV lateral wall, however, negative work did not shown a significant association with percentage LGE in univariate regression analysis (p=0.109). In a multivariate regression model positive work, metabolism and perfusion correlated with percentage LGE (p=0.049, p=0.008 and p<0.001), while peak strain did not (p=0.607).
Conclusions: Septal negative work correlates inversely with septal scar in patients referred for CRT. This finding is probably linked to LBBB, and may be explained by increased stiffness of scar tissue. Myocardial work, but not peak strain, reflects scar in the LV lateral wall. Future studies should explore the assessment of scar in the complete LV and how this relates to CRT response.