ADOPTIVE T-CELL THERAPY (UNIVERSAL KILLERS)
Ideally, efficient tumour-specific effector and memory T cells can be induced by therapeutic vaccination. Nevertheless, in certain cases, active immunization is difficult due to the lack of an effective endogenous T-cell repertoire against the tumour antigens targeted.
T cells can recognize peptides derived from all parts of the cell, including nuclear proteins, which greatly expands the number of potential targets in the tumour cells and offers a large number of new therapeutic opportunities.
Adoptive cell therapy (ACT) involves the administration of large number of highly selected cells with high avidity for tumour antigens.
T cells can be programmed and activated ex vivo to exhibit anti-tumour functions. These cells occur naturally in cancer patients, but are inhibited by numerous immunosuppressive mechanisms in vivo. Adoptive transfer of tumour-specific T cells from tumour infiltrating lymphocytes (TIL) expanded in vitro has already been shown to induce objective cancer regression in patients with metastatic melanoma. A limitation of this approach is the requirement for pre-existing tumour-reactive cells that can be expanded ex vivo and TILs can only be reliably grown from patients with a very limited number of cancer types and mainly melanoma.
In the absence of an adequate level of endogenous tumour-reactive T-cell response, recent clinical studies have shown that it is feasible to compensate for this by engineering a tumour-specific T-cell repertoire by the transfer of genes encoding TCRs or chimeric antigen receptors (CARs). Both of these methods are developed in-house (see below).
UK (PI: S. Wälchli):
The use of the immune system to fight cancer – immunotherapy – has received a tremendous amount of attention recently due to clinical trials where patients with advanced deadly cancer types have actually been cured. One form of immunotherapy uses the patients’ own T cells that are engineered to express cancer-targeting receptors such as chimeric antigen receptors (CARs) or T cell receptors (TCRs) to fight cancer in a process termed adoptive cell therapy (ACT).
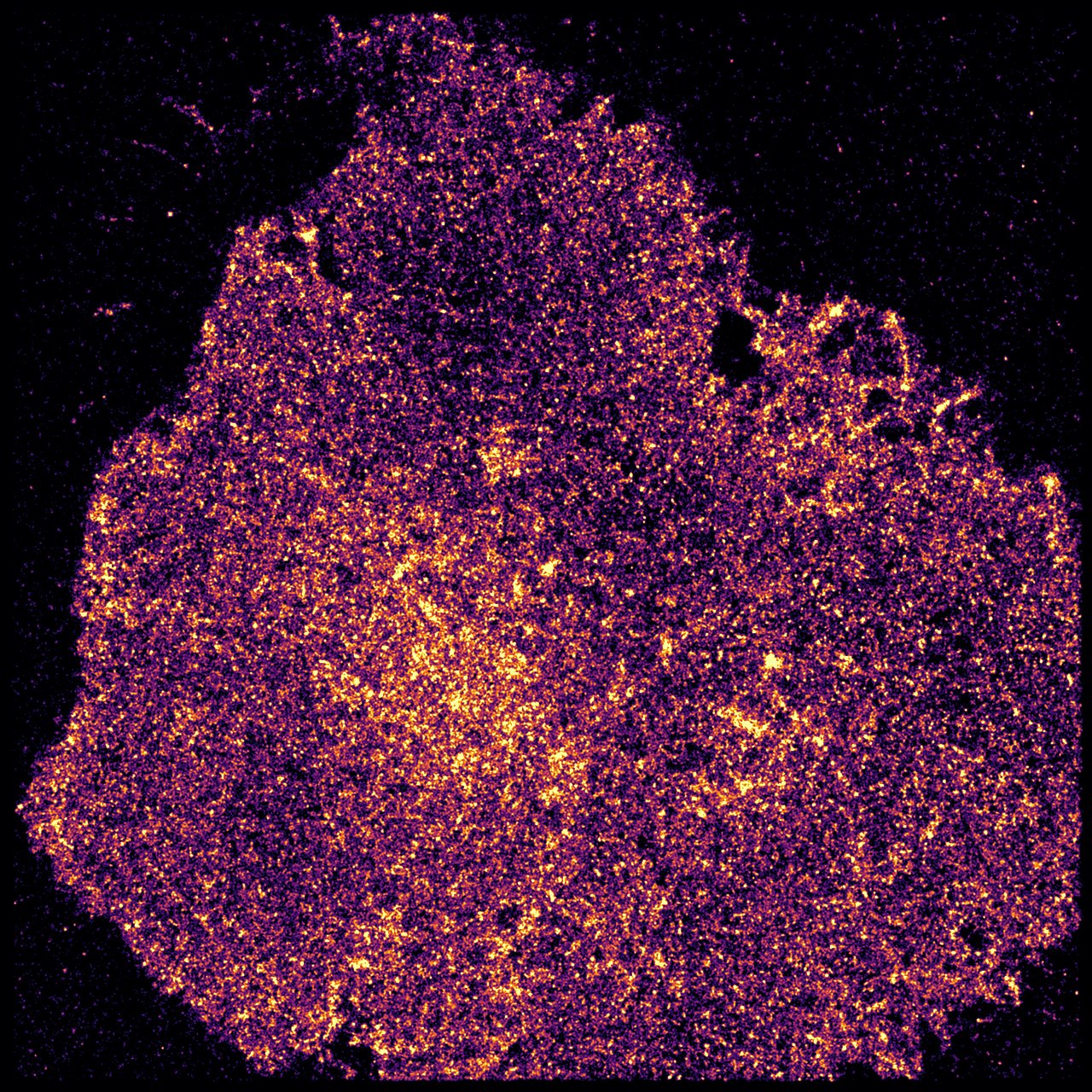
A currently unresolved critical issue with this therapy is that it is highly personal and custom made for each individual patient using the patients’ own T-cells limiting the number of patients that can receive the treatment due to high cost and low production capacity. To solve this critical issue, we have developed a Universal Killer T-cell that is used instead of the patients’ own T-cell and removes the personal aspect of T-cell therapy. The UK-92 cells are non-immunogenic, can be used across patients and efficiently produced in large scale. Furthermore, the UK-92 cells can express virtually any TCR to target any cancer and has the killing capability of normal T-cells.
TCR-based adoptive cellular therapy is a heavy procedure:
Which could be reduced to a few steps by replacing redirected T cells by UK92-TCR:
Received the Inven2 Innovation Prize 2014
Funding from the Norwegian Research Council (BIOTEK2021), Helse Sør-Øst Innovation grant and The Norwegian Cancer Society
