Integrated Cardiovascular Function at the Annual Norwegian Symposium on Heart Research
For the past two decades, NORHEART has been organizing an Annual Symposium covering the latest in cardiac research, with the aim of promoting international quality and to improve career opportunities for PhD students. In recent years Department of Cardiology at Oslo University Hospital and ProCardio Center for Research-based Innovation has engaged in preparations of the meeting.
The symposium is an arena for young researchers to present the studies they are engaged in and a valuable ground for feedback, collaboration and networking. Each year the best abstracts are awarded with prizes to highlight the resent advancements and new knowledge brought about in the field.
Members from the research group Integrated CardioVascular Function impressed with their participation. Deputy group leader Espen Remme sat in the panel for the abstract session on Biomarkers and imaging.
PhD fellow Lars-Egil Hammersbøen, MD won the prize for the best abstract in his session Cardiac function, with the study titled “Non-invasive pressure-volume analysis by three-dimensional echocardiography: a novel method for left ventricular stroke work and efficiency estimation”.
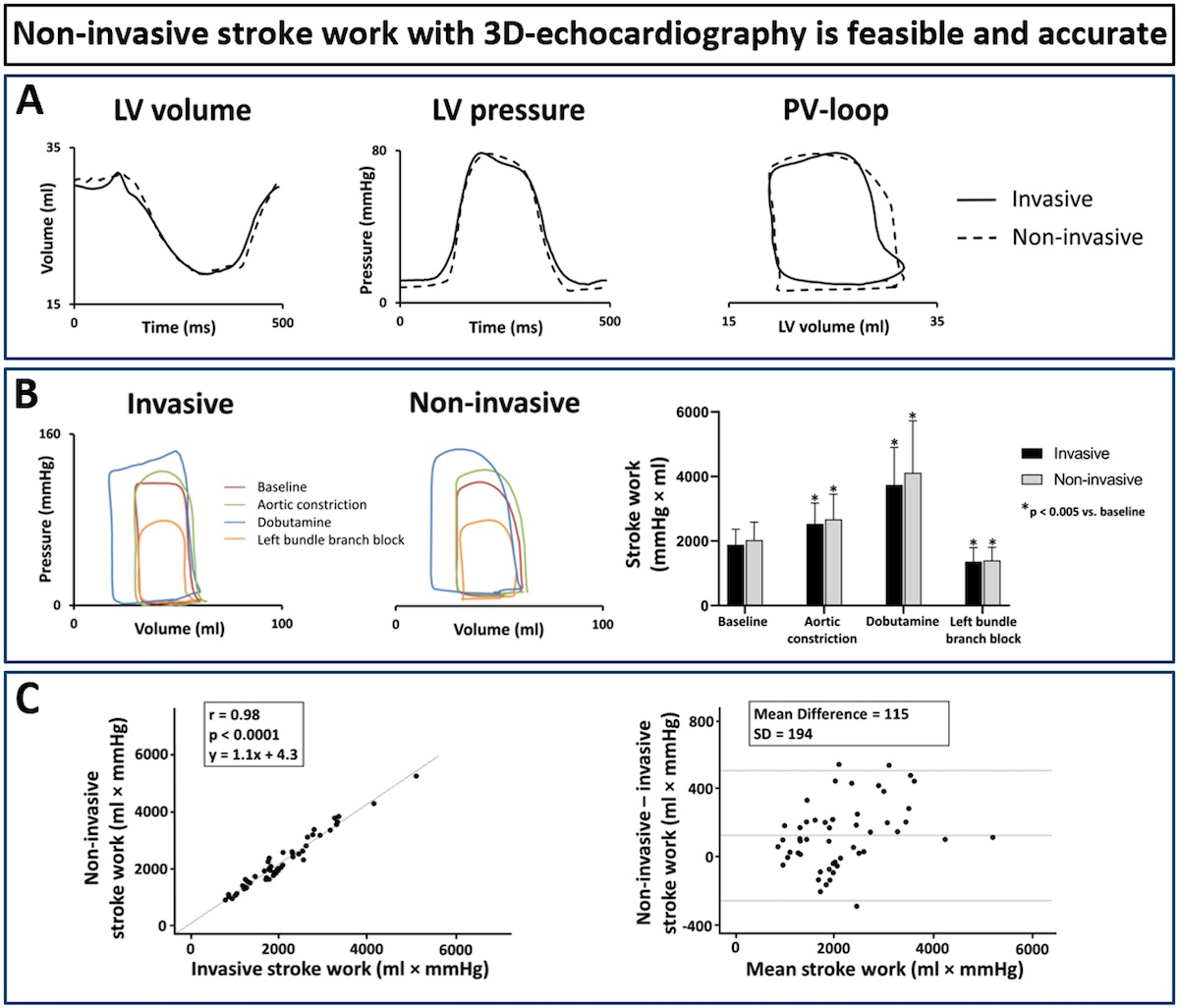
In this study, the investigators used their previously published method to estimate the left ventricular (LV) pressure trace, which was combined with a volume trace from three-dimensional (3D) echocardiography to extract stroke work non-invasively. This non-invasive stroke work was validated against invasive measured pressure and volumes during baseline and different interventions, and showed very good agreement, as can be seen in Figure 1.
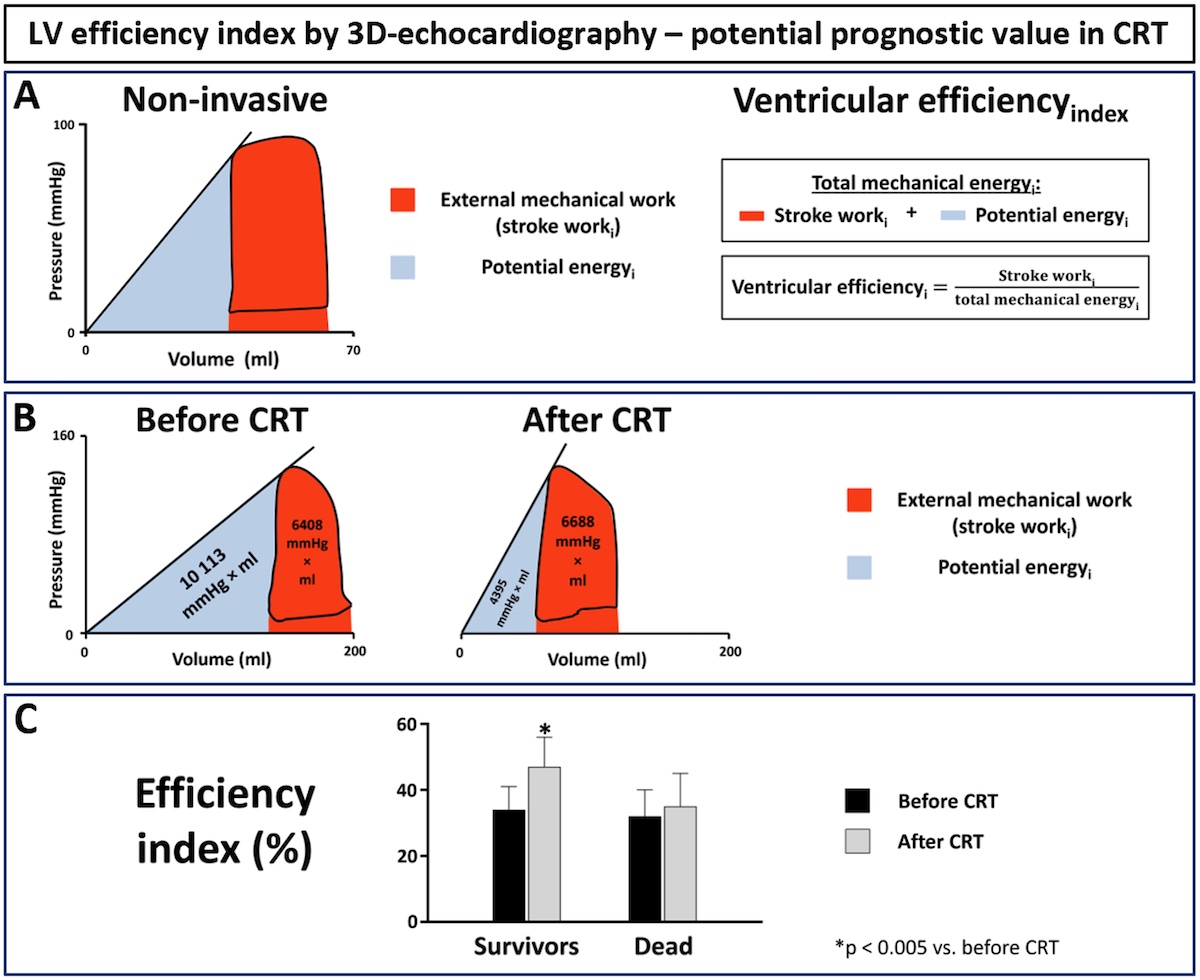
They also proposed a novel index of LV efficiency based on this non-invasive pressure-volume method by 3D echocardiography. A simplified efficiency index was calculated as the ratio of estimated stroke work to estimated total mechanical energy (red area / red + blue areas in Figure 2).
To indicate the clinical potential of the method, they measured this efficiency index in 20 patients who received cardiac resynchronization therapy (CRT). And indeed, patients who survived during follow-up showed significant improvement with CRT, while there was no improvement in patients who died.
These findings show that LV stroke work by 3D echocardiography is feasible and accurate, and that efficiency index may provide prognostic information for CRT patients. Future studies should explore the clinical utility of non-invasive pressure-volume analysis.
PhD fellow Marit Witsø presented the abstract “Reduced left ventricular function after ultra-endurance exercise”, a study to investigate the acute effect on extreme ultra endurance-exercise on left ventricular function. She was awarded with the second prize.
Marit Witsø and Lars-Egil Hammersbøen also presented their research projects at the Annual European Society of Cardiology Congress that took place just prior to the Symposium at Holmenkollen.

Private photo, ESC 2023
Institute leader, Professor Håvard Attramadal sat in the panel for the abstract session Exercise and prevention, together with other prominent researchers from University of Stavanger, NTNU, University of Oslo and University of Bergen.
Head of Department of Cardiology, Professor Thor Edvardsen welcomed everyone to the Symposium and announced the winners of the abstract prizes together with the Director of NORHEART, Professor Kåre-Olav Stensløkken.
Read more on the event and see pictures of all the winners at Annual Symposium 2023: Winners and photos - NORHEART
The winning abstract from the research group Integrated Cardiovascular Function
Non-invasive pressure-volume analysis by three-dimensional echocardiography: a novel method for left ventricular stroke work and efficiency estimation
Lars-Egil R. Hammersboen MDa, b, c, Espen Boe MD, PhDa, b, c, John M. Aalen MD, PhDa, b, Hans Henrik Odland MD, PhDd, Erik Kongsgård MD, PhDb, Manuel Villegas-Martinez MScf, Vetle C. Frostelid MScf, Faraz H. Khan MDa, Ole Jakob Sletten MDa, b, c, Marit Witsoe MDa, b, c, Helge Skulstad MD, PhDa, b, c, Otto A. Smiseth MD, PhDa, b, Marie Stugaard MD, PhDa, c, e, Espen W. Remme MSc, PhDa, f
aInstitute for Surgical Research, Oslo University Hospital, Rikshospitalet, Oslo, Norway; bDivision of Cardiovascular and Pulmonary Diseases, Cardiology Department, Oslo University Hospital, Rikshospitalet, Oslo, Norway; cFaculty of Clinical Medicine, University of Oslo, Oslo, Norway; dDepartment of Cardiology and Paediatric Cardiology, Oslo University Hospital, Rikshospitalet, Oslo, Norway; eVestre Viken Hospital Trust, Ringerike, Norway; fThe Intervention Center, Oslo University Hospital, Rikshospitalet, Oslo, Norway
Introduction: Left ventricular (LV) pressure-volume (PV) analysis is a powerful method to quantify LV function but has limited clinical utility due to the need for invasive pressure and volume measurements. We investigated if LV stroke work can be estimated non-invasively by combining 3D echocardiographic volume measurements with non-invasive pressure curve estimation. Furthermore, we proposed a novel index of LV efficiency calculated from the resulting non-invasive PV-loop and investigated the prognostic potential of this index in patients receiving cardiac resynchronization therapy (CRT).
Methods: In 21 open-chest anesthetized canines, LV volume was measured invasively by piezoelectric crystals and invasive LV pressure by micromanometer. Echocardiography was performed to acquire 3D LV volumes and timings of mitral and aortic valve events. The estimated LV pressure curve was obtained by adjusting the cardiac phases of an LV reference pressure curve to these valve events and adjusting its amplitude to measured peak LV pressure. Invasive and non-invasive stroke work was calculated as the pressure-volume loop area during baseline, aortic constriction, dobutamine infusion and after induction of left bundle branch block by ablation.
Using 3D echocardiographic data from a recent multicenter study, an index of LV efficiency was calculated as the ratio of stroke work to total mechanical energy as shown in Figure 2 panel A, in 10 survivors and 10 non-survivors before and 6 months after implantation of CRT.
Results: The estimated non-invasive and invasively acquired volume and pressure traces and the resulting PV-loop were similar as shown in representative experiments (Figure 1, Panel A and B). The column diagram in Panel B shows that the average stroke work from the animals for the different interventions demonstrating the similarities between invasive and non-invasive stroke work both in value and changes with interventions. Consequently, there was a strong correlation (r = 0.98, p < 0.0001) and good agreement between the non-invasive and invasive stroke work (panel C).
Response to CRT was captured by the marked reduction in left ventricular volumes and hence leftward shift of the PV-loop (Figure 2, Panel B). This corresponded to improvement in efficiency, as stroke work (red) was increased while total mechanical energy area (red + blue) was decreased. As shown in panel C, survival during follow up was associated with marked improvement in efficiency in CRT patients (p < 0.005).
Conclusions: Non-invasive pressure-volume analysis by combining 3D echocardiography and estimated pressure for stroke work evaluation, is feasible and accurate. LV efficiency index calculated from PV-loops by 3D echocardiography may provide prognostic information for CRT patients.