Ovarian carcinomas
Colorectal cancer
Research
Read about the background for our projects:
Large scale genomic instability
We have several projects going on the following material:
Early stage ovarian carcinomas
FIGO Stage I epithelial ovarian cancer:
5-year survival is about 80 %
Material
- Retrospective study
- Paraffin embedded tissue sections
- A total of 305 cases of FIGO stage I epithelial ovarian cancers in Norway collected from 1982 to 1989
- A subgroup of 40 cases are selected from this material for immunohistochemical studies of carbohydrate expression (described later)
- Median follow up time is 9,5 years (range 0,8-12,5 years)
Methods
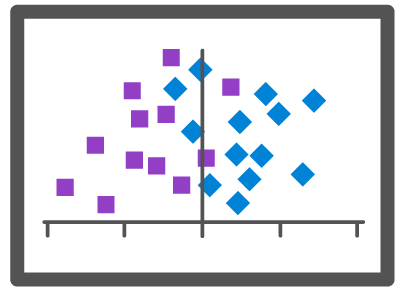
- DNA ploidy is determined using two different methods: flow cytometry (FCM) and image cytometry (ICM)
- Nucleotyping
- Immunohistochemistry
Patient characteristics
- FIGO stage IA 104, IB 19 and IC 182.
- Histological subtype: Serous 66, mucinous 80, endometroid 58, clear celled 69, mixed 10, unclassified 20 and small celled 2.
- Differentiation: Well 131; moderate 47; poor 58 and not graded 69.
Conclusions
DNA ploidy by high-resolution image cytometry is the best predictor of outcome for patients with early stage carcinomas of the ovary, as compared to FIGO staging, histologic subtype, age, dense adhesions and differensiation.
High-resolution image cytometry is superior to flow cytometry in prediction of outcome for patients with early stage carcinomas of the ovary.
| FCM \ ICM | Diploid | Tetraploid | Polyploid | Aneuploid | Sum |
| Diploid | 85 | 29 | 4 | 12 | 130 |
| Tetraploid | 12 | 4 | 15 | 31 | |
| Polyploid | 1 | 1 | |||
| Aneuploid | 9 | 4 | 1 | 54 | 68 |
| Sum | 94 | 45 | 10 | 81 | 230 |
Table 1. Concordance between DNA ploidy classification performed by image and flow cytometry in 230 of the cases of early ovarian carcinoma.
Publications
Gynecological malignancies
Carcinomas of the Fallopian tubes
Material
- Retrospective study
- Paraffin embedded tissue sections
- 47 cases of tubal carcinomas
- FIGO stage 0-1
Methods
DNA ploidy analysis performed by image cytometry.
Preliminary results
- 43 DNA ploidy classifications
- 32 Non-diploid
- 11 Diploid
Germ cell tumors of the ovary
Material
- Retrospective study
- Paraffin embedded tissue sections
- 49 cases of malignant ovarian germ cell tumors
- 20 dysgerminomas
- 17 immature teratomas
- 10 endodermal sinus tumor
- 1 embryonal carcinoma
- 1 chorio carcinoma
FIGO stage
I: 33, II: 6, III: 7 and IV: 3
Follow up > 10 years
Methods
- DNA ploidy analysis performed by image cytometry.
- Comparative genomic hybridization.
Preliminary results
Main findings:
- Most cases were non-diploid 2/3
- None of the patients with diploid, FIGO stage I, IT subtype got recurrence of disease
Publications
Granulosa cell tumors
- Accounts for 3-10 % of malignant ovarian tumors.
- Juvenil and adult.
- 3-10 % malignant recurrence often 10 - 20 years.
- 90 % stage I.
- Staging the only known prognostic factor.
Material and methods
- Retrospective study.
- Paraffin embedded tissue sections.
- Approximately 150 cases.
Advanced stage ovarian carcinomas
5-year survival: regional metastasis < 50 %, distant metastasis 20 %
Scope of these studies
- Examine the DNA ploidy status in relation to
- Hereditary versus sporadic tumors
- Response to treatment
- Comparative genomic hybridization findings
Materials
- Retrospective study
- Paraffin embedded tissue sections
- 100 cases advanced stage ovarian carcinomas mostly serous histological subtype
- 78 cases FIGO stage III ovarian carcinomas mostly serous histological subtypes
- 130 cases advanced ovarian carcinomas
Methods
Results
The results are soon to be evaluated.
Prostate
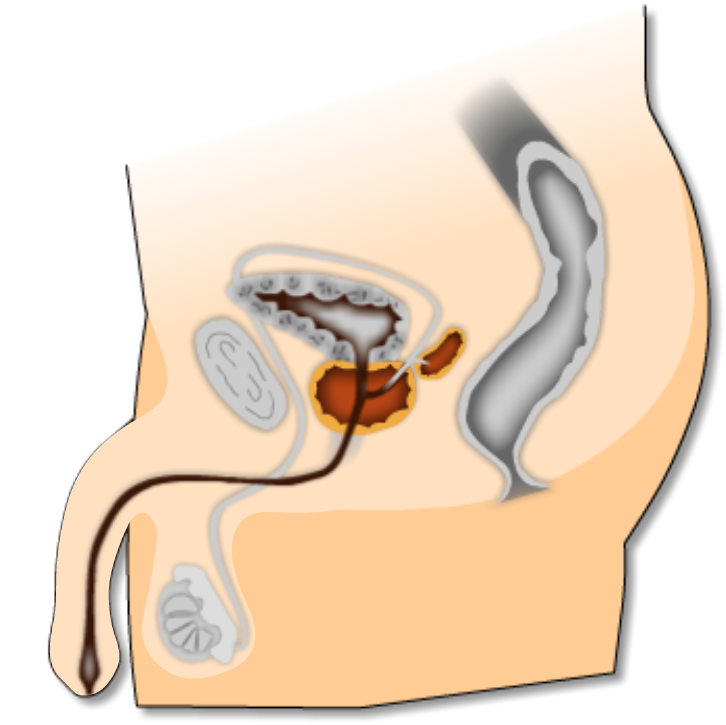
The size of the prostate usually increases after the man has reached the age of 45, and it can be very large in older men (almost 60 grams). In benign prostate hyperplasia, the urethra is compressed and this leads to urination problems. Size and number of ducts and glands increases, and so do the size of the supporting tissues. In prostate cancer (prostate adenocarcinoma), the disease is difficult to discover because the tumour arise in the peripheral glands of the prostate.
Other tissues
* Germinal cell
* Melanoma
* Mola
* Mouse liver
* Pseudomyxom
* Sarcomas
* Tenosynovial tumors
* Testis
* Thyroidea
* Urinary bladder
* Vulvae
Some of the projects on these materials have not yet been ended, so there are no articles published. Methods we have been using are ploidy analysis, texture analysis and immunohistochemistry methods.
Nucleotyping
Nucleotyping are among other an objective measure of nuclei atypi, one of the most important parameters for pathological diagnostics and prognosis. A qualitative analysis of chomatin structure is measured simultaneously with a measure of total amount of chromatin or DNA (depending on staining method) in nuclei. The method give information on the DNA ploidy distribution in addition to traditional nuclei morphometry, and it is sensitive to larger chormosomal aberrations. Of even greater importance is the methods ability to map and quantify functional changes in DNA organisation, that may be induced of larger or smaller mutations. Such changes is to al large ectent subvisual, and will not be discovered using ordinary microscopy. Nucletyping can be described as interphase cytogenetics, that is an interphase variant of chomosomal analysis where we map and describe organisatory and functionally domenes of DNA.
Nucleotyping has a great potential as diagnostic and prognostic/predictive marker in cancer. In opposite to DNA ploidy this method has also a predictive value in cancer at advanced stages.
Nucleotyping is a main priority area at Imaging programme, and we have a number of large studies going on prostate cancer, breast cancer (DCIS and Stage I) and colon cancer, both at The Norwegian Radium Hospital and at institutions in England.
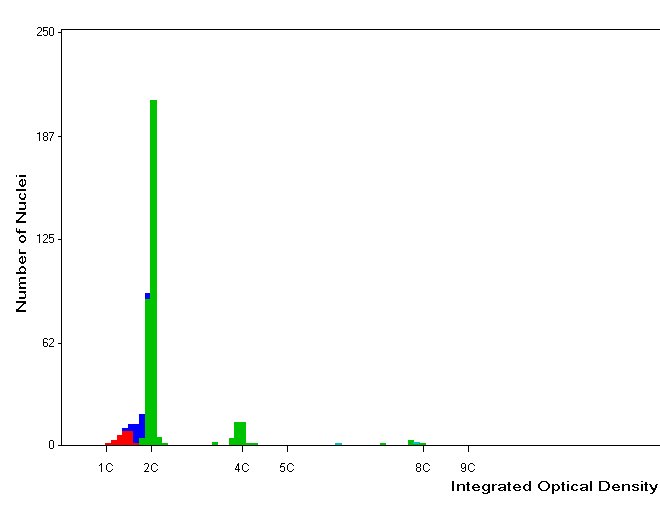
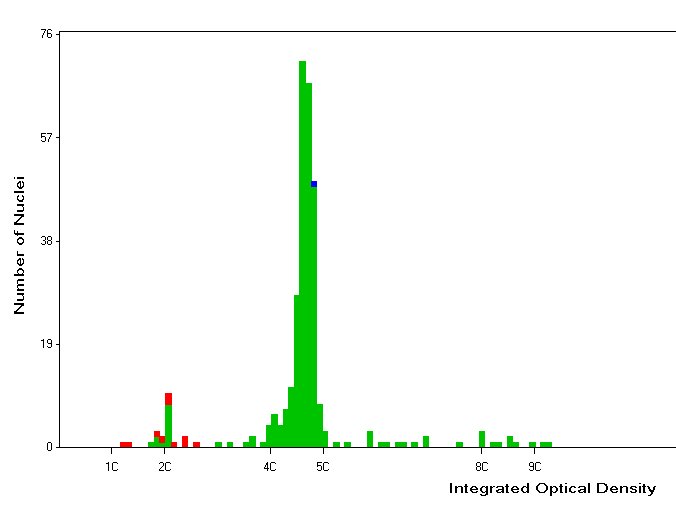
Tetraploid histogram
Aneuploid histogram
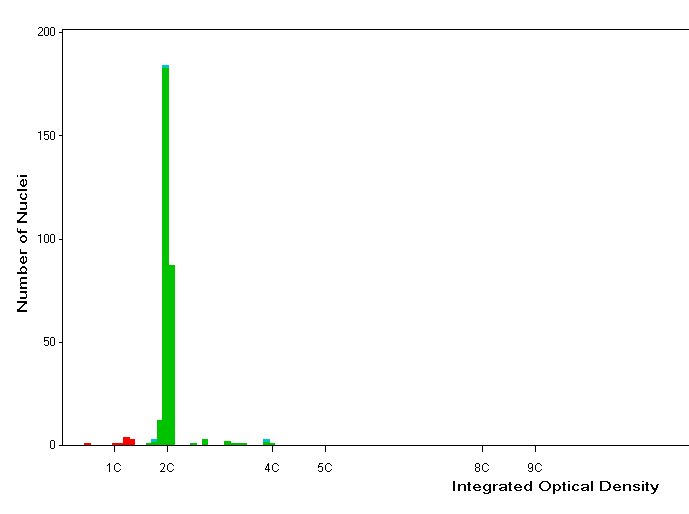
Diploid histogram
DNA-ploidy methods
IMAGE CYTOMETRY
Image cytometry is based on the feulgen tequnique, which is a frequently used staining procedure in biology. The technique is based on Schiffs or Schiffs-similar binding to released aldehyde groups from DNA molecules after hydrolysis by HCl, and thereby enables staining of DNA in situ. The intensity of staining is proportional with the DNA concentration and the amount of DNA in the nucleus is expressed as amount of light absorbed by the feulgen-stain over the entire nucleus. The feulgen reaction is today in use to quantify the DNA ploidy distribution in tumor nuclei.
(The image of each nucleus is transferred from a microscope to a computer through a digital camera. The computer measures the amount of absorbed light as an expression of the amount of DNA.)
FLOW CYTOMETRY
Principles for the method in brief:
A DNA specific fluorocrome binds to DNA. Nuclei is going by a liquid stream, through a optical measuring point. A laser beam splits of photons and the emmited light is measured and thereby expresses the amount of DNA in the tissue sample.
Preparation of samples (in brief) from paraffin embedded tissue :
| Flow cytometry | Image cytometry |
| Sectioning (100mm) | Sectioning (50mm) |
| Deparaffination | Deparaffination |
| Enzyme treatment (pepsine, RNase) | Enzyme treatment (protease) |
| Cytospin centrifugation (monolayer) | |
| Staining with ethidium bromide | Staining with feulgen-schiff |
| Measurements | Measurements |
Advantages and disadvantages of flow cytometry and image cytometry:
| Flow cytometry | Image cytometry | |
| Advantages | Fast | Morphological control |
| Disadvantages | No morphological control | Time-consuming |
Histograms:
| Diploid | Tetraploid | Aneuploid |
Publications
Immunhistochemistry
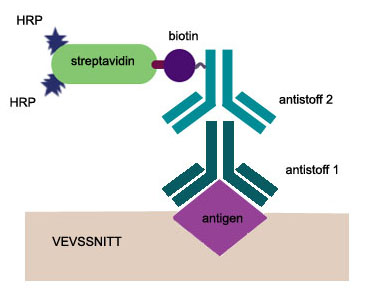
Background
Immunhistochemistry is a powerful technique that allows a researcher to detect molecules within a tissue microenvironment. Protein expression can be studied in relation to tissue or cell compartment, and changes due to either normal or pathologic stimuli can be evaluated. Either direct or indirect methods can be used to detect an antibody bound to an antigen. The direct method uses a labeled reagent, such as a fluorescent tag or an enzyme-linked secondary antibody that binds to the primary antibody. A biotinylated secondary antibody can be used for better sensitivity allowing a tertiary step such as an enzyme-linked avidin or streptavidin to react. While the indirect method involves more assay steps, the amplification process at each step leads to increased sensitivity.
General procedure
· Mount formalin fixed paraffin embedded sections (4 micron) onto silane-coated slides.
· Air dry slides at 37ºC for 24 h.
· Deparaffinize and rehydrate.
· Incubate specimens for 20 minutes in 1-3 drops of serum block. Aspirate serum from slides.
· Immediately add 1-3 drops of pre-diluted primary antibody.
· Incubate for 2 hours. Rinse with PBS then wash in PBS twice for 2 minutes each on a stir plate. Aspirate excess liquid from slides.
· Incubate for 30 minutes in 1-3 drops of biotinylated secondary antibody. Wash as above.
· Incubate for 30 minutes in 1-3 drops of HRP-streptavidin complex. Wash as above.
· Add 1-3 drops HRP substrate mixture. Develop for 30 seconds-10 minutes, or until desired stain intensity develops. Rinse with deionized H2O and transfer to a deionized H2O wash for 2 minutes on a stir plate.
· Counterstain, dehydrate and mount slides
Negative controls underwent similar staining procedure, but with the exclusion of the primary antibody. Positive controls were carcinomas that were shown to be immunoreactive for the studied antigens in preliminary studies.
Interpretation of staining results
The presence of immunostaining in carcinoma cells was evaluated by two independent researchers without knowledge of the clinical outcome. The presence and extent of staining was evaluated, using the following scale: 0, no staining; 1, staining of 1-5 % of tumor cells; 2, staining of 6-25 % of tumor cells; 3, staining of 26-50 % of tumor cells and 4, staining of > 50 % of tumor cells. Staining of both cell membrane and cytoplasm was interpreted as positive.
Large scale genomic instability
CANCER CAN BE VIEWED AS A GENETIC DISEASE
Tumour cells dont usually start out bad. They generally acquire their malignant properties over years or decades, going from benign to invasive to metastatic to lethal, in a process known as tumour progression (Nowell, P.C., Science 194, 23-28, 1976). This process occurs through a series of mutations and chromosomal aberrations that result in the accumulation of aggressive characteristics by the tumour cells (Hanan, D. & Weinberg, R.A., Cell 100,57-70, 2000). Cancer may therefore be viewed as a genetic disease in the sense that genetic (mutations) and epigenetic (organisational, methylations etc.) changes in cells are probable causes of both initiation and progression of cancer.
Findings of single event changes are extremely rare in cancer. In almost all studies, a multitude of genetic changes are observed.
Breast
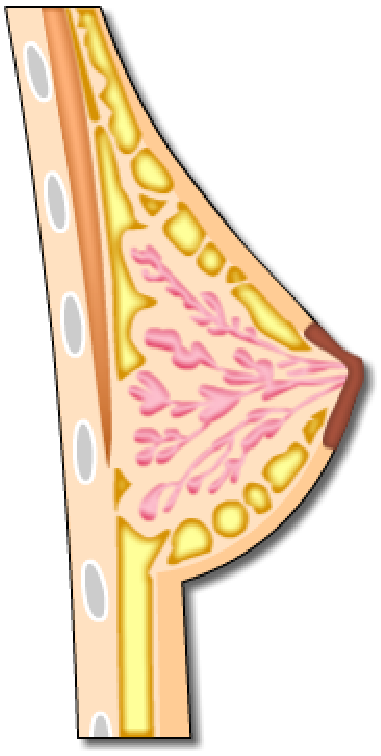
We have two main projects on cancer mammae:
CCIS Study
Ductal Carcinoma in situ represents certain challenges in diagnostics, because around 20 % develop into invasive cancer and there are no certain markers to identify these. We have analysed a number of samples using both DNA ploidy and nucleotyping.
Mammae cancer, stadium I
In this case we have a total of 480 patients with a defined prognosis (good prognosis: no relapse > 7 years after treatment. Bad prognosis: relapse or death of cancer within 4 years). The study is a pilot for DNA ploidy and nucleotyping as a prognostic marker in breast cancer. There are also planned to do a comparison of alternative methods for DNA ploidy measurements (FCM, manual ICM, automated ICM) and S-phase calculations.